By Dr Zoe Drymoussi, Research Manager
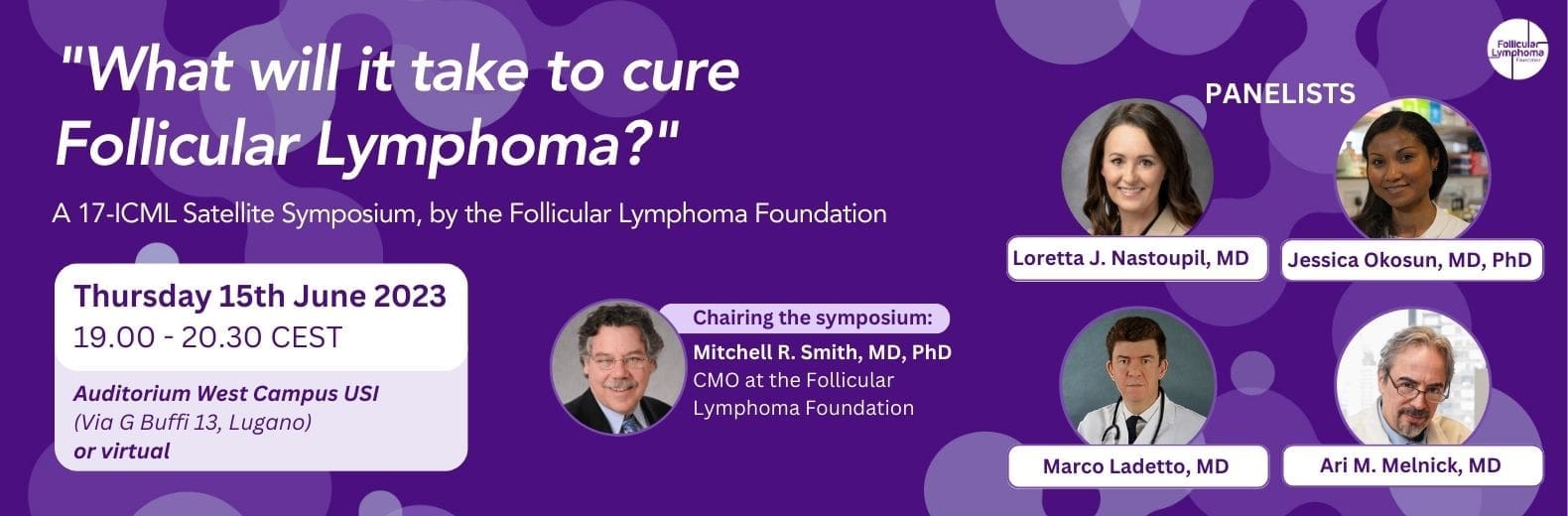
At the recent International Conference on Malignant Lymphoma (ICML), the FLF shone a spotlight on follicular lymphoma (FL), by hosting our very own satellite symposium: “What Will it Take to Cure FL?”.
Dr Mitchell Smith, Chief Medical Officer at the FLF, chaired the session and led the discussion with our expert panel of speakers: Dr Loretta Nastoupil, Dr Jessica Okosun, Dr Marco Ladetto, and Dr Ari Melnick. Together, the panel discussed the remarkable progress in the last twenty to thirty years within basic science, technology, and therapeutics. For FL patients, the new age of cellular therapy (CAR-T, bispecific antibodies) along with the technological advances and deeper understanding of the underlying complex biological mechanisms that cause FL, means that we now have a unique opportunity to change the existing paradigm – to cure FL.
Where are we now?
Dr Nastoupil kicked off the session by exploring some of the newest developments within FL research that she is most excited about – cellular therapies either in the form of CAR-T or bispecific antibody therapies, and where she thinks further progress will be made in the near future. Through the clinical trials in this space, we are seeing encouraging results in the third line setting or later for FL patients. The challenge at the moment is to identify which drugs work best with which patients and also how to improve CAR-T and bispecifics.
Dr Okosun talked about something known as the “common progenitor cell”, or CPC. Researchers think one reason why patients with FL relapse several times may be because there is a residual or reservoir population of cells (the CPCs) that keeps returning to cause the lymphomas. We heard about the opportunities of how we may be able to start targeting CPCs, the more we understand their biology.
Where are we going?
Dr Marco Ladetto shared his work on how we may be able to detect and monitor lymphoma cells at very low levels in a blood test. This will help to inform treatment regimens or even predict how long a patient’s response to a certain treatment will last. This is known as “minimal residual disease”, or MRD, referring to the tiny number of cancer cells remaining in the body, after treatment is finished. Being able to reliably measure MRD in clinical practice has its challenges, and as of now it is not used in routine practice. We heard how efforts are being made to improve these tests, once again taking advantage of our increasing understanding of how FL develops and why it comes back several times in a patient’s journey.
Dr Ari Melnick rounded off the thought-provoking session by focusing on the epigenetic alterations that are important in FL, and showcasing the opportunities of how we could start to target these. Epigenetics refers to the signals inside a cell that turn gene on or off, playing a big role in how cells grow, develop, and die. These factors affect not only the lymphoma cell, but also the immediate environment of the tumour (also known as the tumour microenvironment) – especially the immune response cells which can help control the lymphoma.
Overall, it was a very stimulating and inspiring panel discussion looking across from the basic biology all the way through to how we can translate those learnings into the clinic for FL patients.
When can we start telling patients they are cured?
This is the burning question we put to our panellists. Dr Nastoupil explained how she believes “we probably do cure some patients right now, but we just don’t know how to identify them up front.” In the next five to ten years, the hope is that all the new learnings and deeper understanding of the underlying biology will make clinicians more confident to tell people they are cured – we’re just not there yet.
In Dr Melnick’s words:
I think that the cure is not that far away for many patients. It’s not the same for everyone – there’s no cure–all. It’s important to understand that FL is not a uniform entity. There are many different flavours of FL and they may not all be cured by the same approaches. We’re just starting to understand some of those differences now, but there is an initial understanding and that is taking us in the right direction to eventually get there. A very exciting time.
A big thank you
We would like to thank all our panellists and those who attended in person and virtually. We have had lots of interesting discussions following on from the satellite symposium and will continue to explore the topics covered in more detail. We are grateful for the support we received from our Industry sponsors: an independent educational grant form AstraZeneca, as well as sponsorship support from BeiGene, Novartis and BioInvent International AB. It is still very early days, but we look forward to expanding on this work and are very excited about what the future holds.
Find out more by watching our webinar on this topic!
We hosted a live webinar “How Close Are We to Curing Follicular Lymphoma?” on the 17th of August, 2023. You can hear Dr Loretta Nastoupil and Dr Mitchell Smith being interviewed by Nicky Greenhalgh – the founding member of the “Living with Follicular Lymphoma” Facebook group. Along the theme of “What Does it Mean to Cure FL?” the panellists broke down what the recent advances and developments mean for FL patients, and what we can expect in the near future. The feedback on the day was overwhelmingly positive, so don’t miss out and catch up in your own time!